Angulated
1
View details
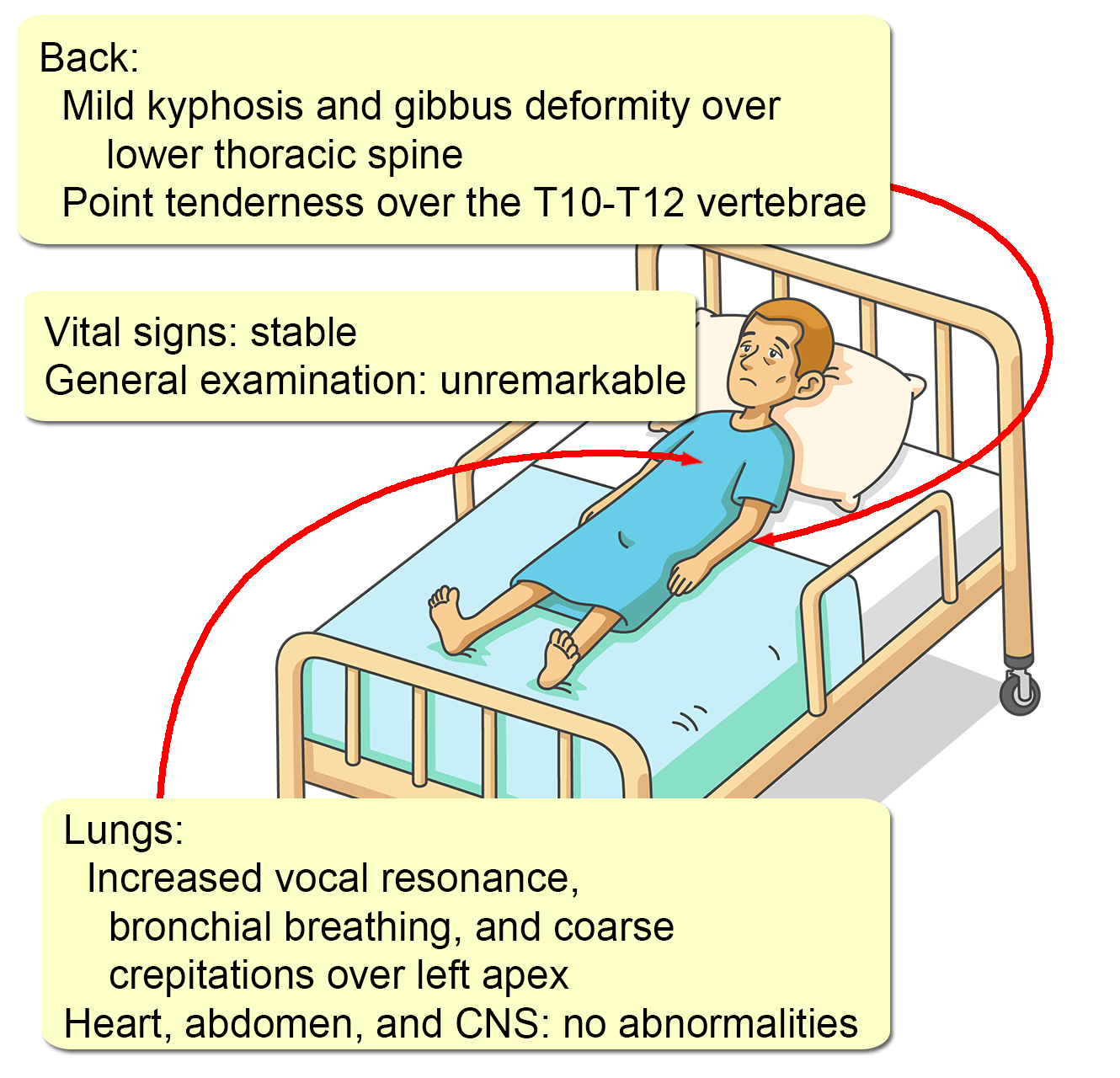
A 35-year-old man presents with upper back pain for two weeks. The pain is constant, dull in nature, without radiation, and aggravated by both weight-bearing and movement. There is no weakness or numbness of the upper or lower limbs. He has had an intermittent nonproductive cough, anorexia, and fatigue for 18 months. He lost 10 kg during the same period. There is no history of trauma, foreign travel, or close repeated contact with animals within or immediately before that period. He was healthy earlier and is not on any medications. His family history is significant for a myocardial infarction in his father at the age of 72 years. He has smoked for 15 years and continues to do so, at an average of two to three cigarettes per day. He only drinks socially and denies using recreational drugs. A full blood count is significant for a Hb of 9.5 g/dL (normal: 11-18), with a MCV of 85 fL (normal: 75-95). His ESR and CRP are 82 mm/1h (normal: <10) and 24 mg/L (normal: <6) respectively. Chest x-rays reveal a heterogeneous opacity in the left upper lobe.