Behind
1
View details
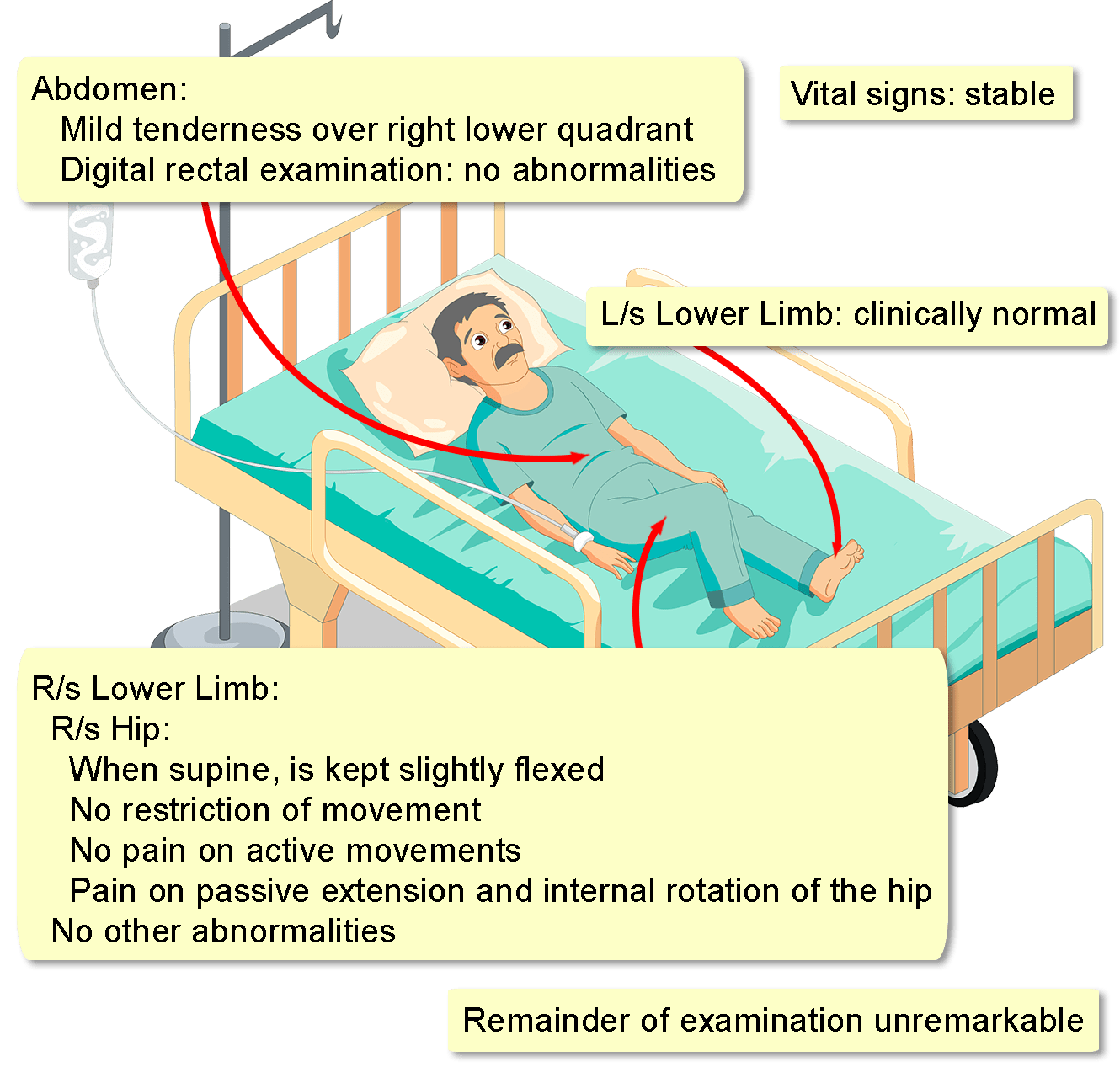
A 55-year-old man presents with right lower quadrant pain for three weeks. The pain is constant and dull, radiates to the right thigh, right hip, and right flank, and is exacerbated by walking and relieved by sitting down.
He experienced an intermittent fever with chills and rigors during the same period, in association with nausea, vomiting, malaise, and a weight loss of 4 kg. There is no history of urinary tract infection or renal stones, and he reports no recent trauma.
His medical history is significant for rheumatoid arthritis for 20 years, which is currently managed with methotrexate and etanercept. His surgical, family, travel, and contact histories are unremarkable, while he is a non-smoker, and only drinks socially.
A complete blood count is significant for a leukocyte count of 15,000/mm3 (normal: 3,500-10,500), with 90% neutrophils (normal: 40-80). Serum electrolytes, renal and liver function tests, a clotting profile, a random plasma glucose assay, and an abdominal ultrasound are all normal.