Heartbreaker
1
View details
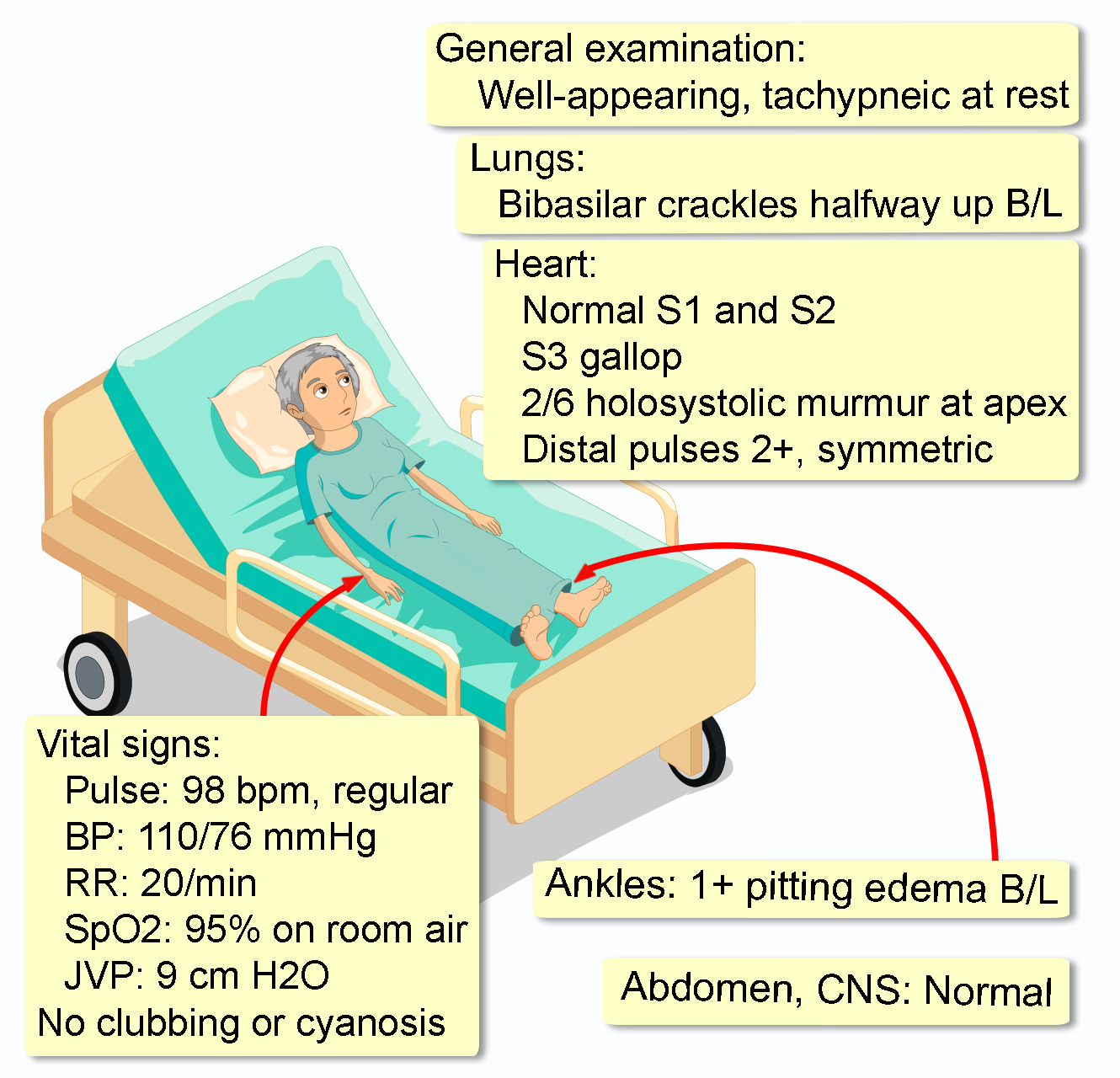
A 58-year-old woman presents to her primary care physician with a 3-month history of progressive shortness of breath and fatigue. She initially noticed dyspnea only with strenuous activities like brisk walking but now feels breathless walking up a single flight of stairs. She requires two pillows to sleep comfortably at night and has noticed swelling in her ankles towards the end of the day. She denies chest pain, palpitations, or fainting spells.
Her medical history is notable for stage II-A breast cancer diagnosed 6 years ago. She was treated with a modified radical mastectomy followed by adjuvant chemotherapy with doxorubicin and cyclophosphamide. She subsequently completed a 5-year course of anastrozole. Her oncologist follows her regularly, and she is in remission. She has no personal history of hypertension, diabetes, or coronary artery disease. She quit smoking 6 years ago after her cancer diagnosis (15-pack-year history) and drinks alcohol socially.
Initial laboratory studies are as follows:
WBC: 7,500/mm3 (4,500-11,000)
Hemoglobin: 13.1 g/dL (12.0-16.0)
Hematocrit: 39% (36-46)
Platelets: 250,000/mm3 (150,000-450,000)
Na+: 138 mEq/L (136-145)
K+: 4.2 mEq/L (3.5-5.1)
Cl-: 101 mEq/L (98-107)
HCO3-: 25 mEq/L (22-29)
BUN: 24 mg/dL (7-20)
Creatinine: 1.2 mg/dL (0.6-1.1)
TSH: 2.5 mIU/L (0.4-4.0)