Ruptured
1
View details
An 82-year-old woman is brought to the emergency department by ambulance after collapsing at home. She regained consciousness en route but complains of severe, tearing back pain radiating to her left flank. Her medical history is significant for hypertension, hyperlipidemia, and chronic obstructive pulmonary disease (COPD). She is a former smoker with a 40-pack-year history. She has no known history of abdominal surgery. Medications include lisinopril, atorvastatin, and daily aspirin. She has no known drug allergies. Initial vital signs recorded by paramedics showed a blood pressure of 85/50 mmHg and a heart rate of 110 bpm. Two large-bore IV lines were placed, but no fluids have been administered yet.
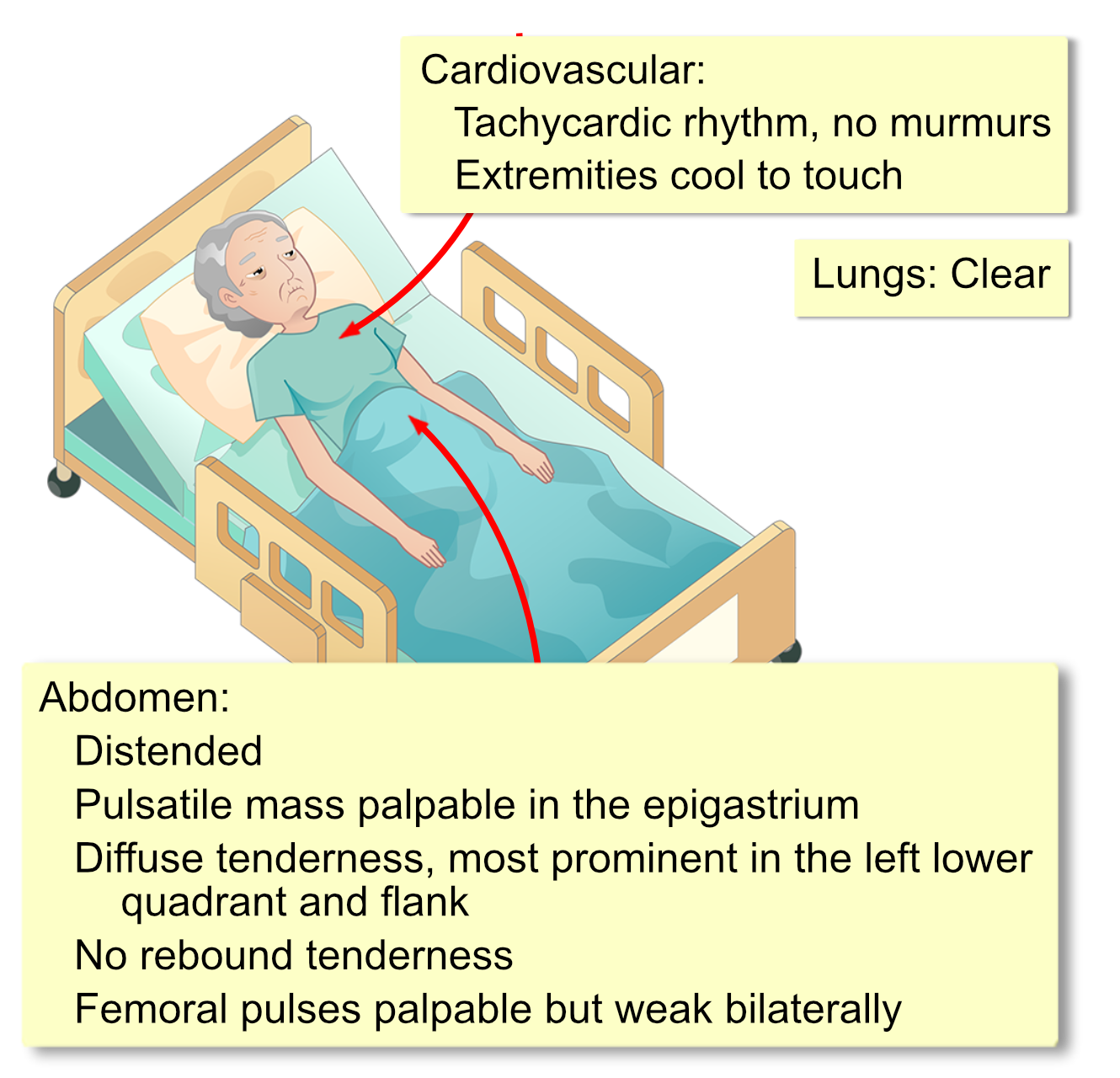
Her temperature is 98.0o F (36.8o C), heart rate is 155 bpm, respirations are 24/min, blood pressure is 88/55 mm Hg, and O2 saturation is 96% on room air. She is pale, diaphoretic, and anxious but oriented.
Initial laboratory studies are as follows:
WBC: 14,500/mm3 (4,500-10,000)
Hemoglobin: 9.8 g/dL (12.0-15.5)
Hematocrit: 30% (37-47)
Platelets: 180,000/mm3 (150,000-400,000)
PT: 13 seconds (11-15)
aPTT: 28 seconds (25-40)
Na+: 138 mEq/L (136-146)
K+: 4.2 mEq/L (3.5-5.0)
Cl-: 102 mEq/L (95-105)
HCO3-: 20 mEq/L (22-28)
BUN: 28 mg/dL (7-18)
Creatinine: 1.1 mg/dL (0.6-1.1)
Lactate: 3.5 mmol/L (0.5-1.0)
Glucose: 140 mg/dL