Sore Subject
1
View details
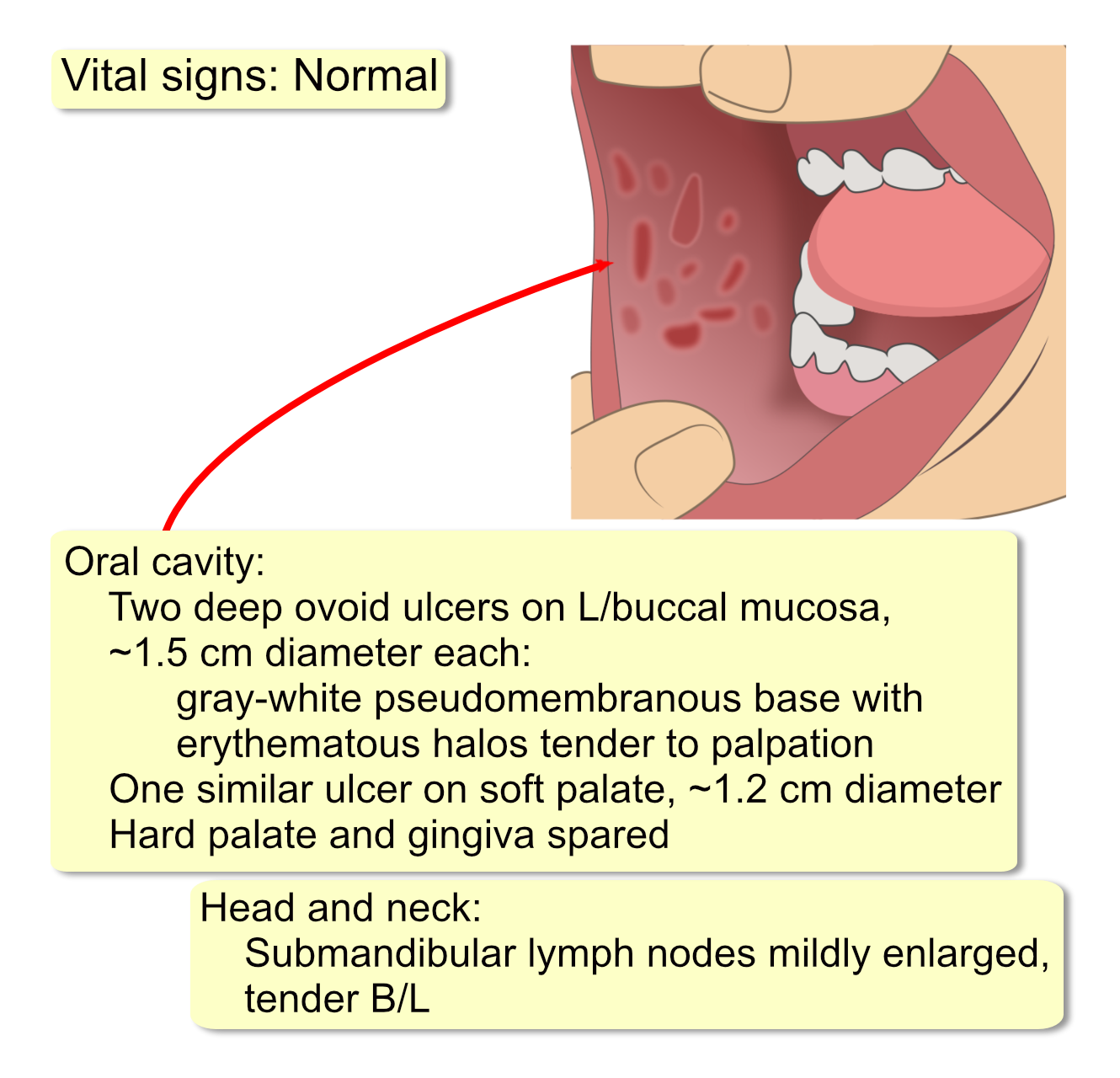
A 22-year-old female graduate student presents to the clinic with extremely painful mouth sores for the last two weeks. She has a one-year history of smaller, recurrent oral ulcers. These typically occur every one to two months and resolve within 7-10 days. However, the current episode is her most severe. The large, deep ulcers make it difficult to eat or speak, which has resulted in a 5-pound weight loss. She notes a tingling sensation at the sites for about a day before the ulcers appeared. Her family history is positive for her mother and sister having “canker sores.” She denies any genital ulcers, eye pain or redness, skin rashes, joint pain, diarrhea, or fevers. She is a lifelong non-smoker and drinks alcohol occasionally. Initial laboratory studies are as follows:
WBC: 7,500/mm3 (4,500-11,000)
Hb: 13.5 g/dL (12.0-15.5)
Platelets: 280,000/mm3 (150,000-450,000)
ESR: 25 mm/hr (0-20)
CRP: 1.2 mg/dL (<1.0)