Stuck
1
View details
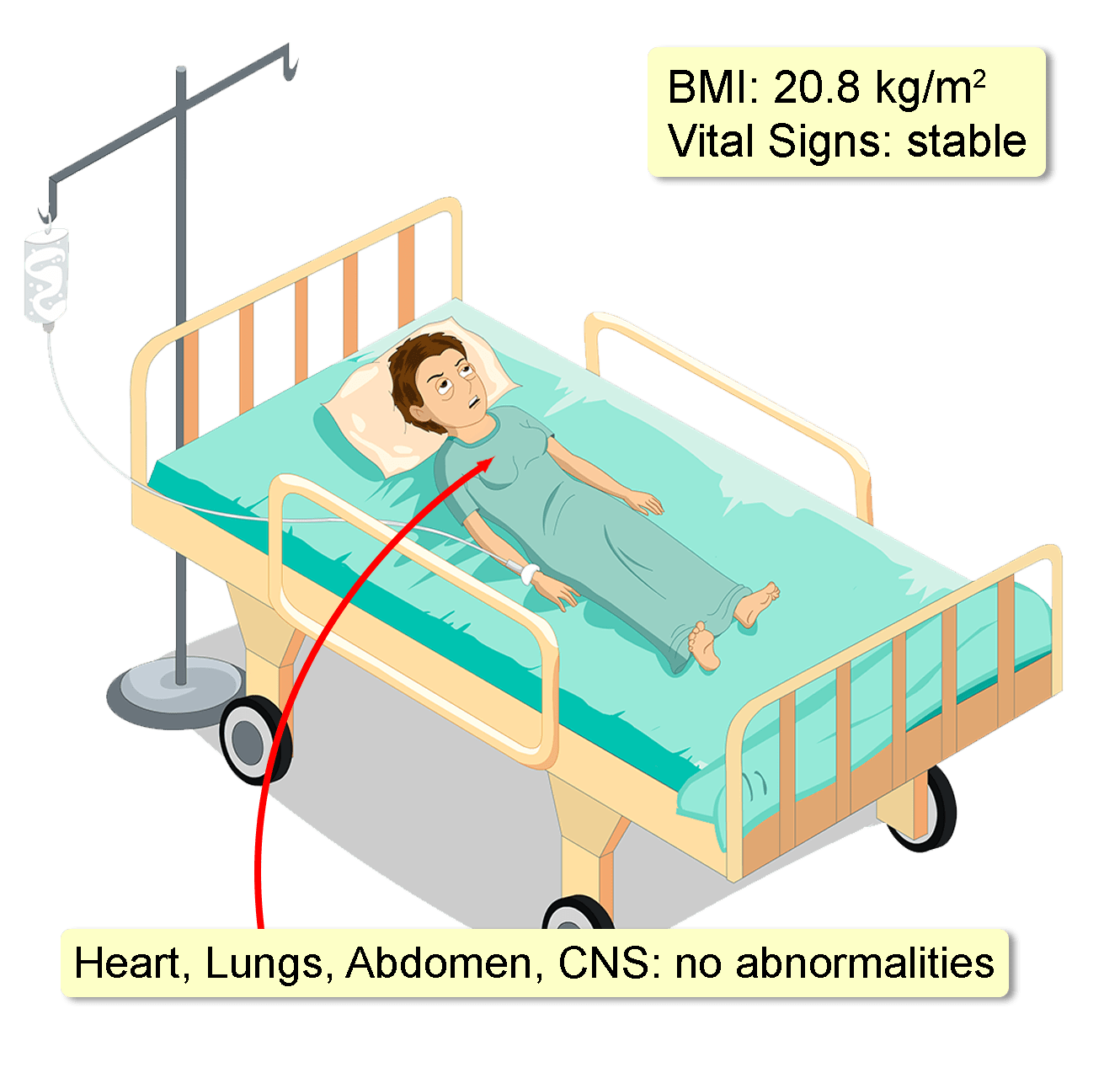
A 52-year-old woman presents with worsening intermittent “burning” chest pain for one year. The pain does not radiate; and is not exacerbated by exertion or lying down. Her primary care physician prescribed a two-week course of omeprazole one month ago, but her symptoms were unchanged. Careful questioning reveals mild dysphagia to both solids and liquids for the last six months, together with some episodes of saliva regurgitation while lying down. This feeling is worst in her upper chest. She also lost 5 kg of weight during the same time period. Her medical history is only significant for uncomplicated mild hypertension for 4 years. This is well controlled on amlodipine 10 mg daily. She does not smoke and only drinks socially. A full blood count, two 12-lead ECGs, and an exercise stress test have been ordered recently. All were normal.