Under Pressure
1
View details
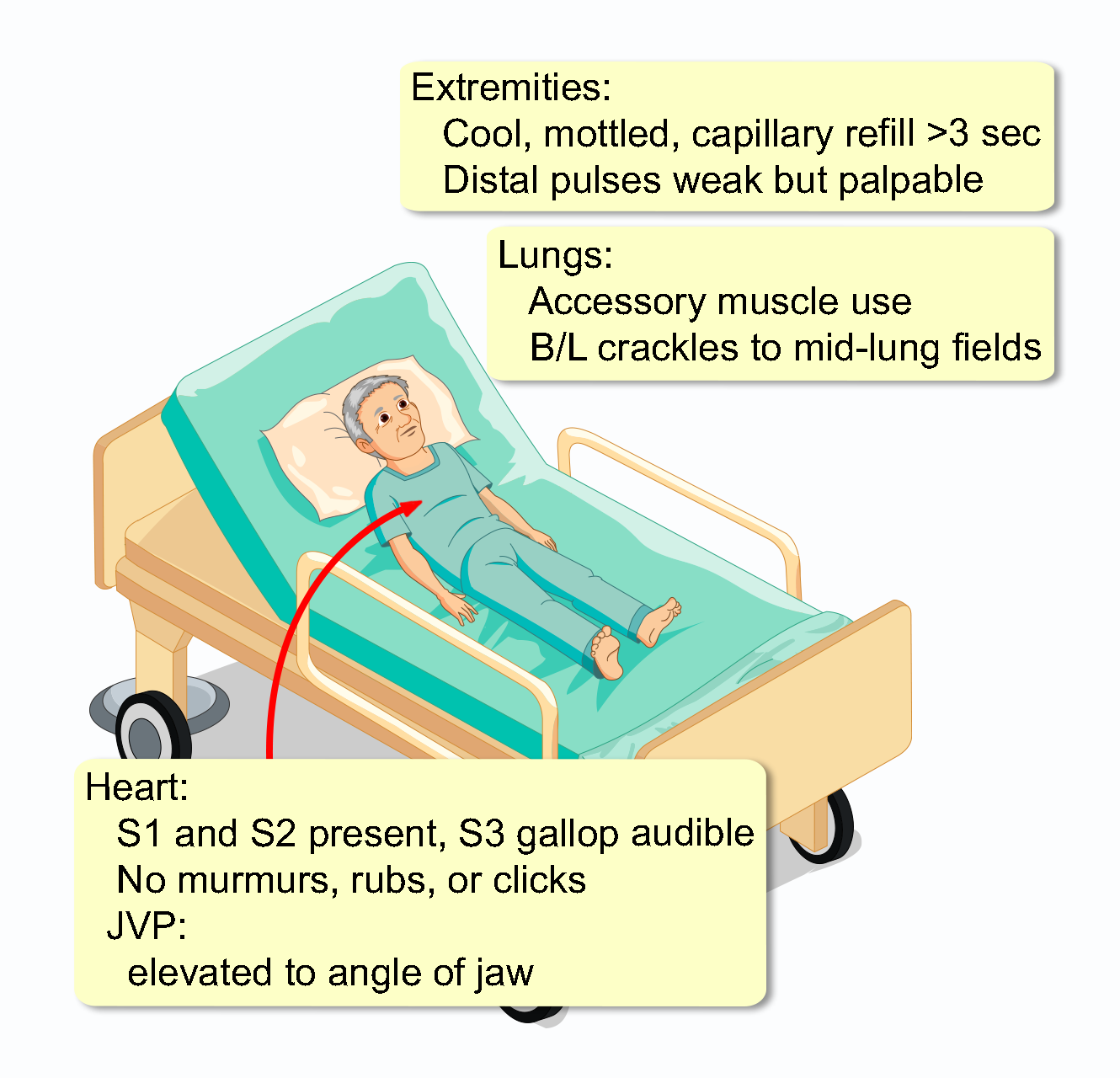
A 68-year-old man with a history of hypertension and hyperlipidemia presents to the emergency department. His chief complaint is 3 hours of severe, crushing substernal chest pain. The pain radiates to his left arm and is associated with profound diaphoresis, nausea, and shortness of breath. He denies any recent illness, trauma, or similar previous episodes. His medications include lisinopril and atorvastatin. He has no known drug allergies. He is a former smoker with a 20 pack-year history but quit 10 years ago. He drinks alcohol socially. On arrival, he was alert and oriented. However, he has become progressively more lethargic and confused over the last 15 minutes. His pulse is 110 and regular, BP is 85/60 mmHg, RR is 24/min, and SpO2 is 88% on room air. He is markedly diaphoretic.
Initial laboratory studies are as follows:
WBC: 14,500/mm³ (4,500-11,000)
Segmented neutrophils: 85% (54-62)
Hemoglobin: 14.1 g/dL (13.5-17.5)
Hematocrit: 42% (41-53)
Platelets: 250,000/mm³ (150,000-400,000)
Na⁺: 138 mEq/L (136-146)
K⁺: 4.2 mEq/L (3.5-5.0)
Cl⁻: 101 mEq/L (95-105)
HCO₃⁻: 18 mEq/L (22-28)
Glucose: 160 mg/dL (70-100)
BUN: 30 mg/dL (7-18)
Creatinine: 1.6 mg/dL (0.6-1.2)
Lactate: 4.5 mmol/L (0.5-1.0)