Waterlogged
1
View details
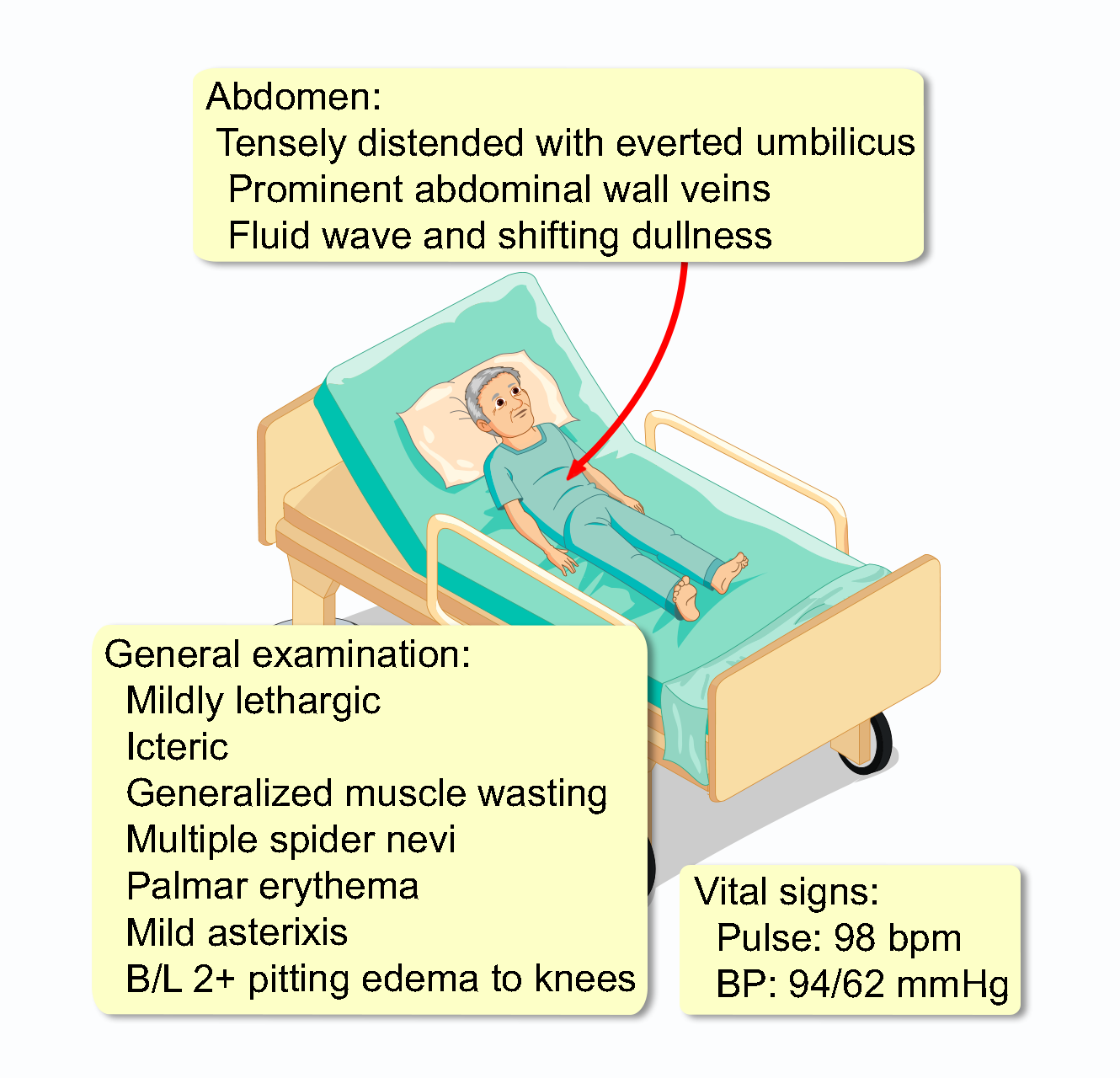
A 64-year-old man presents to the emergency department with a 2-week history of worsening abdominal distension, shortness of breath, and a 15-pound weight gain (~6.8 kg). His past medical history is significant for cirrhosis secondary to chronic hepatitis C (treated and cured with antivirals 5 years ago) and a long history of alcohol use disorder, in sustained remission for 2 years. He has had ascites for the past 3 years, which has been managed with diuretics and a low-sodium diet. He reports compliance with his current diuretic regimen of spironolactone 400 mg daily and furosemide 160 mg daily. However, his urine output has decreased over the last month. He denies fever, chills, or new abdominal pain. His appetite is poor, and he has noticed increasing muscle wasting in his arms and legs.
Initial laboratory studies are as follows:
WBC: 7,500/mm3 (4500-10,000)
Hemoglobin: 10.8 g/dL (13.5-17.5)
Platelets: 85,000/mm3 (150,000-400,000)
INR: 1.6 (0.8-1.2)
Na+: 132 mEq/L (136-146)
K+: 4.8 mEq/L (3.5-5.0)
BUN: 30 mg/dL (7-18)
Creatinine: 1.4 mg/dL (0.6-1.2)
Total Bilirubin: 3.2 mg/dL (0.1-1.0)
Albumin: 1.8 g/dL (3.5-5.5)
ALT: 45 U/L (10-40)
AST: 88 U/L (12-38)